Abstract

BACKGROUND
The rate of major arterial and venous thrombosis in primary myelofibrosis (PMF) and post-ET (PET) and post-PV (PPV) secondary myelofibrosis has been evaluated in a limited number of studies.
In the present paper we describe the clinical epidemiology of thrombosis in a large series of patients with overt PMF and PPV/PET MF looking at the rate and risk factors. Moreover, we report findings on thrombosis rate in two cohorts of patients treated with Hydroxyurea (HU) or Ruxolitinib (Ruxo).
METHODS
Patients were registered in the European Registry for Myeloproliferative Neoplasms (ERNEST). This project, promoted by the European LeukemiaNet, is coordinated by FROM - Foundation for Research, Papa Giovanni XXIII Hospital, Bergamo (Italy) and supported by Novartis through a research collaboration . Patients were diagnosed in 6 Centers from Italy, Spain and Sweden, between Jan, 2001 and Dec, 2012, with the required follow-up information.
Patients (n= 1010) with PMF (n=584, 59%), PET-MF (n=207, 20%) and PPV-MF (n=219, 21%) were evaluated for incident thrombosis as primary endpoint. Considering death as a competitive event, uni-and multivariate analyses were performed by applying Fine & Gray competing-risk regression models.
RESULTS
After a median follow-up of 3.8 years (IQR: 1.8-7.1) from diagnosis, 108 thromboses (10.7%) occurred, for an overall incidence rate of 2.0% pts-yr (95% CI: 1.7-2.5). Arterial thromboses were found in 50 patients (46.3%) including cerebral (n=21, 19.4%), myocardial infarction (n=13, 12.0%) and peripheral events (n=9, 8.3%). Venous thromboses were 58 (53.7%), of which 25 (23.0%) were DVT ± PE and 11 (10.2%) were splanchnic. Thrombosis rate was 1.91, 1.60 and 2.79% pts-yr in PMF, PET-MF and PPV-MF, respectively.
In univariate analysis, factors significantly associated with an increased thrombotic risk in PMF were age (p=0.013) and the presence of the JAK2 mutation (p=0.003); in addition, a significant higher proportion of PMF patients at low and intermediate-1 vs intermediate-2 or high risk IPSS score, had thrombosis during the follow-up (p=0.008). In multivariate analysis, only JAK2 mutation retained statistical significance (SHR=3.12, 95% CI: 1.40-6.94, p=0.005). Conversely, neither in univariate nor in multivariable analysis, significant risk factors were not found.
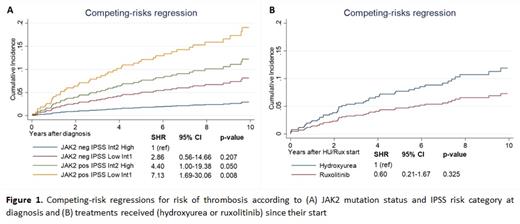
To investigate the possible interaction of IPSS score and JAK2 mutation we created a model whose results are presented in Fig. 1A: the cumulative incidence function (CIF) of thrombosis was significantly lower in patients with JAK2 wild-type and intermediate-2 or high IPSS score (CIF: 4% projected at 10 years; SHR=1 [reference category]), while patients at the highest risk for thrombosis harbored JAK2 mutation and were categorized at low or intermediate-1 by IPSS score (CIF: 20% projected at 10 years, SHR=7.13, p=0.008). Of note, thrombosis had a significant impact on mortality. After adjusting for sex, age, year of diagnosis, type of MF and IPPS, HR was 1.51, (95% CI. 1.15-1.98, p=0.003).
The influence of drug exposure to incident thrombosis was investigated in two cohorts of 559 consecutive patients exposed to HU (n=470) or to Ruxo (n=89), median treatment 2.6 and 3.0 years, respectively. HU- compared to Ruxo-treated patients were older (median age 67 vs. 63 years, p=0.001), more frequently triple negatives (12% vs. 2%, p=0.036), less splenomegalic (spleen length >10 cm: 30% vs. 88%, p <.001) and less symptomatic (49% vs. 79%, p=0.031). Of note, median time from MF diagnosis to therapy start in Ruxo group was 4 years, whereas patients started HU at MF diagnosis. In 56 of 89 Ruxo-treated patients (62.9%), the drug was given after a prior HU therapy. The thrombosis rate from the time of initiation of therapy was 2.40% pts-yr (95% CI 1.78-3.24) under HU and 1.28% pts-yr (95% CI 0.48-3.41) under Ruxo (CIF curves in Fig. 1B). In multivariate analysis corrected for MF type, DIPPS at first drug administration, JAK2 mutation and time from MF diagnosis, exposure to Ruxo showed a non-significant trend towards a protection of approximately 70% compared to HU (SHR=0.33, 95% CI: 0.08-1.32, p=0.117).
CONCLUSION
IPSS score, in addition to the survival risk assessment, may be useful, if associated with the JAK2 mutation, to recognize patients at vascular risk and to suggest appropriate anti-thrombotic prophylaxis. The trend towards a benefit of Ruxo, compared to HU, warrants a study in larger case series.
Barbui: AOP Orphan: Membership on an entity's Board of Directors or advisory committees, Research Funding; Novartis: Membership on an entity's Board of Directors or advisory committees, Research Funding. Passamonti: Janssen: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Novartis: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Celgene: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; BMS: Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; AbbVie: Speakers Bureau. Vannucchi: Incyte: Membership on an entity's Board of Directors or advisory committees; Novartis: Membership on an entity's Board of Directors or advisory committees, Other: Lectures; Celgene: Membership on an entity's Board of Directors or advisory committees, Other: Lectures; AbbVie: Membership on an entity's Board of Directors or advisory committees, Other: Lectures.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal